Prostatitis is an inflammatory process associated with inflammation of the prostate gland (prostate) in men. Most often, this disease occurs in men older than 30 years. This disease causes pain in the lower back, perineum or pelvis, is accompanied by a violation of normal urination, and in severe forms leads to erectile dysfunction and serious problems in the relationship with a partner.
About a quarter of cases in couples suffering from infertility are precisely the causes of the male factor affecting the impossibility of conception. Male infertility is a violation of the quality of sperm and their quantitative content in the ejaculate.
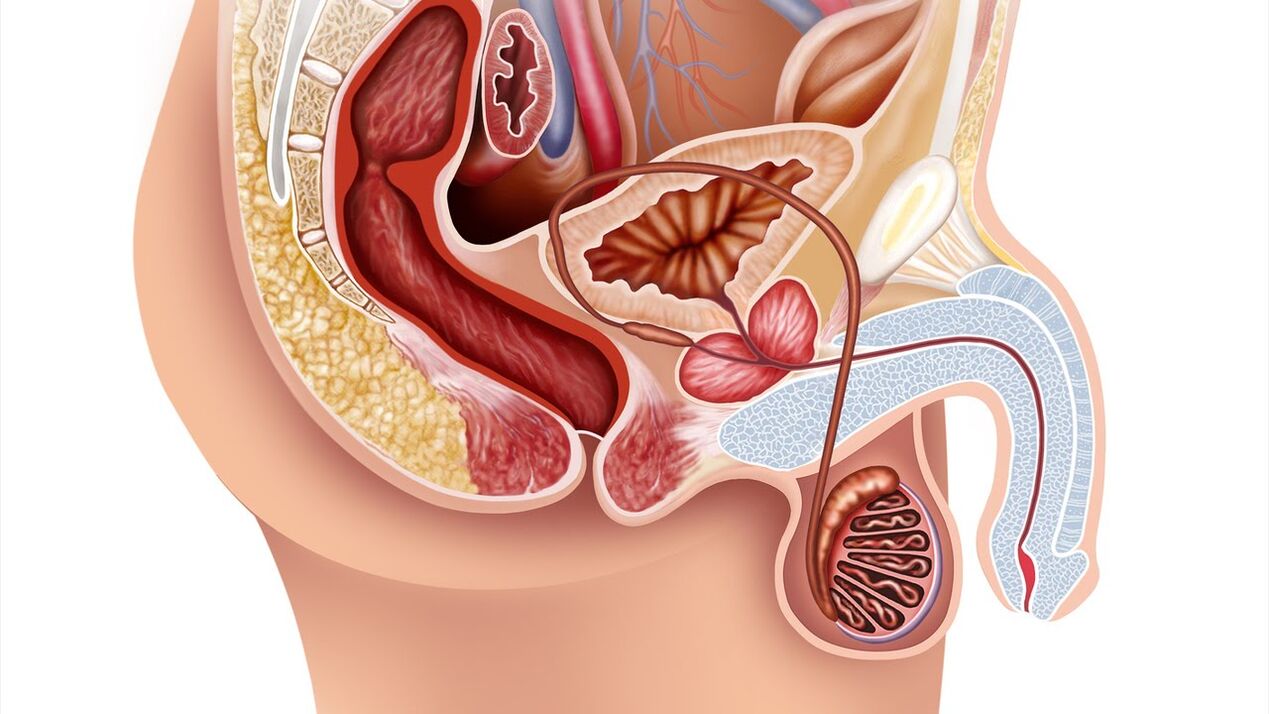
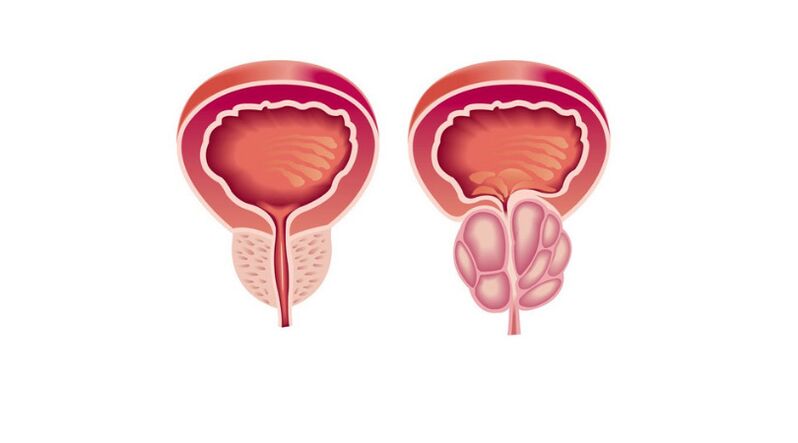
The prostate (prostate) refers to the male reproductive system. It is chestnut-shaped, located in front of the rectum, under the bladder and surrounding the urethra (urethra). When the prostate becomes inflamed, it compresses the urethra, further causing problems with urination. The main function of the prostate is to produce a secretion (fluid) that is part of the semen and dilutes it, which ensures normal sperm motility.
Prostatitis is very common in the practice of a urologist. It can occur suddenly or gradually, constantly and over a long period of time (chronic prostatitis). The chronic form of this disease is more common than the acute form. Chronic prostatitis ranks fifth among the twenty most important urological diagnoses.
Since prostatitis is an active focus of infection in the body, it requires mandatory treatment, even if its symptoms do not bother you.
Reasons for the development of prostatitis
The list of causes that provoke inflammation of the prostate is very diverse:
- Diseases of the genitourinary system (cystitis, urethritis, pyelonephritis);
- sexually transmitted infections (trichomoniasis, gonorrhea);
- Infections associated with pneumonia, influenza, tonsillitis, furunculosis;
- chronic constipation, forcing a man to regularly exercise;
- sedentary lifestyle and irregular sex life, leading to stagnation of the secret;
- urinary retention - a swollen bladder increases pressure on the prostate;
- frequent hypothermia (or overheating);
- pelvic injuries;
- hormonal disorders that weaken the immune system.
Very often the occurrence of prostatitis is caused by pyogenic microbes: E. coli, streptococci and staphylococci, mycoplasma, candida fungi, trichomonas, tubercle bacillus. They multiply very quickly and destroy prostate tissue, resulting in inflammation.
In most cases, the occurrence of prostatitis provokes an infection that penetrates the prostate gland through the urethra. It happens that it enters the body through the blood or lymph, starts from the bladder or rectum.
Important! A decrease in immunity is very dangerous for a patient with chronic prostatitis, since the prostate quickly becomes inflamed due to fatigue, stress, lack of sleep, malnutrition and other adverse factors.
With a sedentary lifestyle and the lack of a constant sex life, the blood supply to the pelvic organs deteriorates, which leads to oxygen starvation in the prostate tissue and congestion. A stagnant secret is an ideal environment for the development of pathogenic microorganisms that cause inflammation.
Types and forms of prostatitis
Depending on the cause of the disease, prostatitis is divided into types and forms:
By type they are distinguished:
Bacterial prostatitis- Inflammation from infection. Bacterial prostatitis occurs in both young and older men.
stasis prostatitis- Inflammation due to stagnation of secretion. It develops in men with a sedentary lifestyle who do not have a regular sex life. This form can quickly be supplemented by infection, and then the stagnant process will be complicated by the bacterial form.
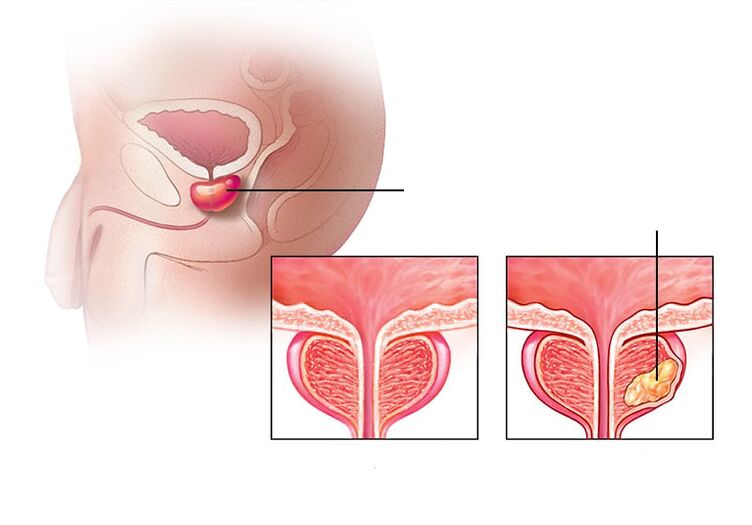
Calculated prostatitis- Stones form in the prostate. Untreated chronic prostatitis can cause this complication. This disease affects older men who have not followed the advice of a urologist.
Depending on the type of flow, they are distinguished:
Acute form of prostatitis- This is an inflammation of the prostate caused by an infectious agent, characterized by the appearance of edema and purulent foci in the tissues. 30-58% of men of childbearing age (30-50 years) face such a diagnosis.
Chronic form of prostatitischaracterized by persistent or recurrent urogenital symptoms caused by bacterial infection of the prostate. The chronic form accounts for 10% of all cases of prostatitis.
Symptoms of prostate inflammation
GeneralSymptoms of prostate inflammationare:
- pain in the lumbar region;
- discomfort during intestinal motility;
- pain in the perineum or pelvic area;
- Disorders in the work of the lower urinary tract.
The acute stage of prostatitis is accompanied by a general intoxication syndrome. This disease is characterized by a sharp manifestation of symptoms with a vivid clinical picture:
- a sharp increase in body temperature, chills, nausea, vomiting and malaise;
- pain syndrome and chills in the joints and muscles;
- an enlargement of the prostate and the occurrence of discomfort in the perineal area;
- frequent urination and urinary retention.
Against the background of individual inflammatory processes, a purulent-septic disease that affects the blood can develop. In such a situation, the patient needs urgent hospitalization: with sepsis, the treatment of prostatitis should be carried out exclusively in the clinic.
At thechronic prostatitis of a bacterial natureSymptoms are usually absent, so treatment begins only when an infection in the urinary system is detected, which manifests itself against the background of a complication of the disease. In this case, you can observe the following:
- pain during ejaculation;
- the appearance of blood in the ejaculate;
- the presence of discharge from the urethra;
- Erectile dysfunction can develop.
If the examination did not reveal that chronic pain is caused by pathologies in the prostate, in this case it ischronic nonbacterial prostatitisor the so-calledChronic Pelvic Pain Syndrome. With this disease, the quality of life of a man is significantly reduced, as it leads to various disorders of a psychological and sexual nature:
- increased fatigue;
- a feeling of helplessness;
- erectile dysfunction;
- painful ejaculation;
- pain after intercourse, etc.
Similar symptoms can also occur with other urological diseases, so it is impossible to diagnose prostatitis based on symptoms alone. For example, disturbances and pain in urination occur with prostate adenoma, cystitis, various oncological tumors in the urogenital organs, etc.
Diagnosis of prostate inflammation
Having noticed the first signs of an inflammatory process of the prostate, the patient should immediately contact a doctor - a urologist. The doctor needs to exclude many diseases with similar manifestations and determine what kind of disease they belong to.
To confirm that the patient does not have other diseases (for example, appendicitis, oncology, inflammatory processes in the bladder and kidneys, prostate adenoma), the doctor must conduct the necessary examinations:
- anamnesis (questioning of the patient);
- general inspection;
- rectal examination;
- studying the mystery of the prostate;
- Analysis for sexually transmitted infections;
- Ultrasound examination of the prostate, scrotum and pelvic organs.
At the appointment, the urologist should discuss with the patient the duration of the clinical manifestations of the disease, the localization and nature of the pain (for example, in the perineum, scrotum, penis and inner thigh), characteristic changes in sperm (the presence of pus andBlood).
The doctor diagnoses chronic bacterial prostatitis if the symptoms last at least three months.
The survey includes:
- Digital rectal examination of the gland to determine the degree of prostate enlargement and its consistency.
- Analysis of prostate secretion, urine and/or ejaculate.
- Identification of a urogenital infection.
- Urodynamic study.
- Ultrasound examination of the urinary tract (kidneys, prostate, bladder with determination of residual urine).
- Cultural examination of prostate secretion and microscopy of different portions of urine and prostate secretion.
- Androflor is a comprehensive study of the microbiocenosis of the urogenital tract in men by PCR, which will determine the qualitative and quantitative composition of the microflora.
After identifying the cause of the disease, the doctor will recommend a course of treatment. It must be remembered that standard methods can detect infection, which ultimately leads to prostatitis, only in 5-10% of cases.
It is imperative that the patient undergo thorough diagnostics, because the success of the treatment depends on the accuracy of the results.
treatment of prostatitis
When a urologist makes a diagnosis, establishes the cause and form of prostatitis, he must prescribe treatment.
The leading role in the treatment of this disease is attributed to drug therapy:
Antibacterial Therapy
At the first stage of therapeutic therapy it is necessary to eliminate inflammation. Antibiotics are the main treatment for acute bacterial prostatitis and are recommended for chronic bacterial prostatitis. The doctor will choose an antibacterial drug depending on which bacteria caused the disease. The patient needs to take oral antibiotics in a course for 4-6 weeks. Chronic or recurrent prostatitis takes longer to resolve. With very severe manifestations, hospitalization may be required, during which intravenous treatment with antibiotics is performed. Usually this happens with acute bacterial prostatitis.
Treatment with alpha1 blockers
If you have trouble urinating, your doctor will prescribe alpha1 blockers, which make it easier to urinate and relax your prostate and bladder muscles. Muscle relaxants relieve the pain caused by swelling of the prostate, which puts pressure on nearby muscles. Nonsteroidal anti-inflammatory drugs help relieve the painful syndrome.
Also, the doctor may prescribe auxiliary drugs: biostimulants, extracts of various plants and insects in the form of rectal suppositories. Unfortunately, the use of drugs alone in the treatment of prostatitis is still insufficient.
In the treatment of this disease, the principles of sequence of action must be observed. Treatment of prostatitis is always complex.
Physiotherapy in the treatment of prostatitis
In the categories of chronic prostatitis, you can additionally use physiotherapeutic methods:
- Massage of the prostate (prostate);
- laser therapy;
- microwave hyperthermia and thermotherapy;
- electrical stimulation with modulated currents using skin or rectal electrodes;
- Acupuncture (acupuncture).
Alternative methods such as hirudotherapy (treatment with medicinal leeches) are sometimes used to treat prostatitis, but the effectiveness and safety of this method has not been proven.
Introduction of stem cells
Cell therapy (stem cell injections) is a promising method of treating prostatitis today, it is at an early stage of development. With regard to the injection of stem cells into the prostate, one can only have hypotheses about its mechanisms and empirical data from individual research groups.
Surgical treatment of prostatitis
Surgical methods are used to treat complications of prostatitis (abscess and suppuration of seminal vesicles).
The treatment of chronic pelvic pain syndrome requires separate consideration. Asymptomatic inflammatory prostatitis does not require treatment.
Diet and lifestyle in prostatitis
Prostatitis does not require a special diet, but eating plenty of vegetables, lean meat, and dairy products will help improve bowel function. It is necessary to enrich your body with a sufficient amount of fiber, foods rich in vitamin E (wheat germ, corn oil, etc. ), and replace sugar with natural honey. Proper nutrition with inflammation of the prostate helps improve bowel function and reduce the likelihood of a recurrence or speed up recovery. The patient must be limited to drinking coffee, excluding alcohol, drinking plenty of fluids and adhering to a healthy lifestyle.
Preventive measures to prevent prostatitis
If a man leads the right way of life: he eats right, does sports, then his chances of developing chronic prostatitis are very small. Refusal of bad habits and casual sex are the prevention of this disease.
Important! There are primary and secondary preventions to prevent the development of prostatitis in men.
Primary- aim to prevent the occurrence of the disease. It depends on a balanced diet, physical activity, timely treatment of infectious diseases of the body and regular protected sexual intercourse, etc.
Secondary- aims to prevent the recurrence of existing chronic prostatitis and provides for regular examination by a urologist and preventive treatment with multivitamins, restorative drugs and sports.





























