Prostatitis is inflammation of the prostate that is common these days.
The prostate is a male organ and therefore the disease is also purely male.
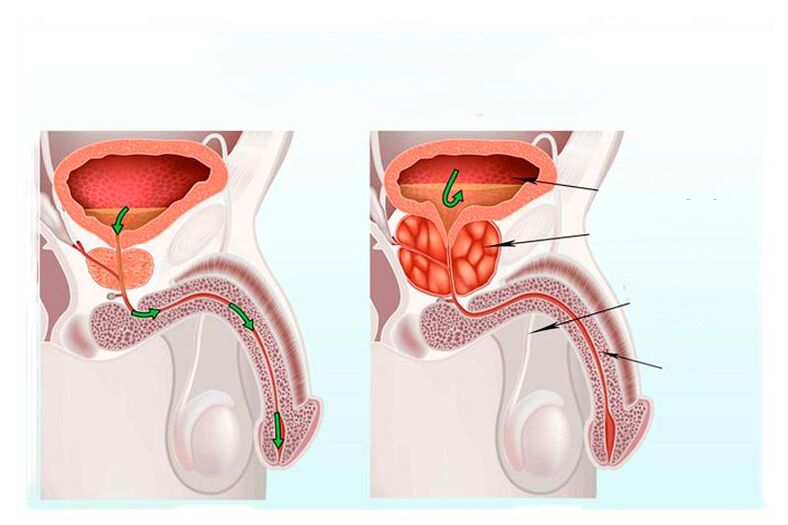
Why is a prostate needed? The prostate is responsible for the following functions:
- produces a liquid part of the sperm with the muscles of the bladder neck;
- produces an internal sphincter;
- converts testosterone to dihydrotestosterone.
The prostate, or simply the prostate, is located under the bladder, the urethra runs through the prostate and therefore the prostate is located around the urinary tube. And because the prostate enlarges during inflammation, it compresses the urinary canal and makes it difficult to urinate. Men over forty years of age very often suffer from prostatitis. This is a consequence of the malfunction of the genitourinary system.
Factors provoking the development of prostatitis:
- Hypothermia;
- Infectious diseases;
- Alcohol and tobacco consumption;
- Trauma and hormonal imbalances;
- sedentary work;
- Urinary retention.
Prostatitis is divided into several types:
- Acute bacterial prostatitis: occurs when the prostate tissue is damaged by Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus, etc.
- A large number of these bacteria are members of a healthy microflora and live on our skin and in the stomach. However, when they get into the tissues of the prostate, they cause inflammation. The main symptoms of acute bacterial prostatitis are nausea and pain in the groin and lower back, frequent visits to the toilet and pain when urinating, poisoning of the body and a decrease in the quality of erections, and signs of blood in the urine.
- Chronic bacterial prostatitis: occurs due to violations of the genitourinary system or the presence of infections in organs.
- The symptoms of chronic prostatitis are expressed in pain during urination and frequent urge, discomfort in the groin, blood in the semen and an increase in body temperature of 0. 5 to 1 degrees Celsius.
Chronic bacterial prostatitis occurs when lifting heavy objects with a full bladder, as a result of which urine enters the prostate, spasms of the pelvic muscles, so - increased pressure in the prostate, injury. Symptoms include painful urination, and only laboratory tests can tell an infectious difference.
Chronic prostatitis
Chronic prostatitis is a dangerous disease that, unlike prostatitis, brings with it a number of unclear questions. What is Chronic Prostatitis? Chronic prostatitis is the presence of inflammation in the prostate, which is characterized by a series of tissue changes and dysfunction of the prostate, the activity of the male reproductive system. Chronic prostatitis is one of the earliest diseases affecting the male reproductive system. The classification of chronic prostatitis is divided into several subspecies:
- acute bacterial prostatitis;
- chronic bacterial prostatitis;
- chronic abacterial prostatitis;
- inflammatory prostatitis with an increase in leukocytes in the secretions of the prostate;
- non-inflammatory process without an increase in leukocytes;
- Inflammation of the prostate without symptoms that is detected by chance.
Infection caused by neurovegetative disorders causes and provokes the development of chronic prostatitis. Hemodynamic disorders lead to a decrease in immunity due to autoimmune and biochemical processes. Factors in the development of chronic prostatitis are lifestyle features that cause infection of the genitourinary system, frequent hypothermia and sedentary work, irregular sex life or the constant presence of a urethral catheter are also dangerous. Important and dangerous pathogens of the disease are also disorders of the immune system, cytokines and bacteria with a low molecular weight polypeptide nature that influence the functional activity of immune cells.
One of the main reasons for the development of non-inflammatory forms of chronic prostatitis is the dysfunction of the pelvic floor.
Chronic prostatitis symptoms
Chronic prostatitis is pain and discomfort, urination dysfunction, and sexual dysfunction. The presence of pain in the pelvic area, perineum and groin. Pain is often observed in the anus and scrotum. Sex life is disturbed and libido also decreases, but these signs are not observed in all patients. Chronic prostatitis is interchangeable, symptoms worsen and then subdued. In general, the symptoms of chronic prostatitis are similar to the stages of the inflammatory process. Pain in the scrotum and groin is characteristic of the exudative stage, as well as frequent urination, accelerated sperm eruption and painful erections. The alternative stage is characterized by pain in the suprapubic part, normal urination, and with accelerated semen outbreak, no pain is observed during erections. In the proliferative stage we can also observe increased urination and the process of ejaculation is slightly delayed. At the stage of sclerosis of the prostate, in addition to cicatricial changes, the patient has pain in the suprapubic part, frequent urination, and ejaculation of the semen is slowed or absent. It should also be borne in mind that the stages and disorders described above do not always occur and do not occur for everyone.
To diagnose chronic prostatitis, a number of tests and laboratory tests will help, since very often the disease is asymptomatic. Tests are also important to help the doctor identify the intensity of symptoms, pain, and urinary disorders. The laboratory examinationchronic prostatitis helps diagnose chronic prostatitis and possible infection of the prostate with atypical bacterial and fungal flora and viruses. If the secretions of the prostate with an increased number of leukocytes do not have bacterial growth, an analysis for chlamydia is necessary. Microscopic examination helps reveal the number of leukocytes and mucus, trichomonas and epithelium in the secretion of the urethra. The secret obtained after massaging the prostate is used for bacteriological examination, and based on its results, the nature of the disease is determined. It is also important to conduct an immunological study, the results of which will help determine the stage of the disease and monitor the effect of treatment. Instrumental examination of chronic prostatitis will help determine the stage and form of the disease, further monitoring it in the course of treatment. Ultrasound examination makes it possible to study the size and volume of the prostate, the structure of the cyst and sclerotic changes in the organ, the degree of expansion and density of the contents of the seminal vesicles. Muscle and pelvic floor myography as well as information on suspected neurogenic urinary tract diseases. An X-ray study will be done to clarify the cause of the outbreak and the course of further treatment for chronic prostatitis. Computed tomography of the pelvic organs is performed to rule out pathological changes in the spine and pelvic organs. Diagnosis, as the exclusion of a disease unsuitable for symptoms, helps determine the nature of the pathological process: with inflamed processes in other organs; with diseases of the rectum; with sexual dysfunction; in neuropsychiatric disorders such as depression or reflex sympathetic dystrophy.
Chronic prostatitis treatment
Treatment for chronic prostatitis should be consistent and comprehensive. First, it is necessary to change the patient's usual way of life and thinking. Also eliminate the influence of harmful factors such as smoking and alcohol consumption, hypothermia. In this way we stop the further development of the disease and soon provoke a recovery. Already in the preparation phase for the treatment, adherence to the diet and the establishment of a sexual life play an important role. The next main course in treating the disease is the use of medication. Such a correct approach to the treatment of chronic prostatitis will not only help fight the disease, but also increase the effectiveness of treatment at each stage of the development of prostatitis. Chronic prostatitis does not generally require hospitalization, but in severe cases of chronic prostatitis, inpatient treatment is more beneficial and effective than outpatient treatment. Treatment with drugs leads to good blood circulation in the pelvic organs, brings hormones and the immune system to normal levels. In such cases, antibacterial drugs and immunomodulators, vasodilators and prostate massage are used. The antibacterial use of drugs is the basis for the treatment of chronic prostatitis. Unfortunately, this therapy has been shown to be effective, but not for all types of prostatitis. Antibacterial treatment is effective for chronic bacterial prostatitis, and empirical antibacterial treatment is used for chronic bacterial prostatitis.
At the moment, local physical treatment is very important. Physiotherapy using laser, mud, and electrophoresis is considered to be the most effective. The electromagnetic radiation is based on an anti-congestive and bacteriostatic effect. The low-energy laser therapy stimulates the microcirculation in the tissues of the prostate, and the laser therapy also has a bio-stimulating effect. In the absence of contraindications, therapeutic prostate massages are used.
Surgical interventions are increasingly used in the treatment of prostatitis as the disease affects more and more young men. An indication for an operation can be a sclerosis of the seminal tubercle. Such patients often consult a doctor with signs of a lack of sexual sensations and ejaculation. In such cases, a resection of the seminal tubercle is performed. The operation is also used for sclerosis of the bladder and prostate.
Symptoms of prostatitis
Very often men with prostatitis complain of a fever and high body temperature. Even if the temperature measured under the arm is normal, the temperature in the anus is very often elevated. Pain in the lower back, lower abdomen, perineum, anus, and scrotum also serve as a signal to see a doctor. Even more often when urinating, cramps and a burning sensation occur during urination. There is a deterioration in the general condition, weakness, pain in muscles and bones, severe headache.
If the prostate is inflamed in men, it is difficult to urinate, and this is often associated with urinary retention. Constipation, which occurs as a result of compression of the rectum by an enlarged gland, is characteristic of the disease.
Treatment of prostatitis
Before starting treatment, it is necessary to accurately establish the diagnosis. The minimum manipulations that should be performed are measurement of the temperature in the anus, diagnosis and palpation of the inguinal perineum of the lymph nodes, a general clinical blood test and a general urine test are also required. You will also need to take swabs from the urethra and bacterioscopy of urine and sediment. In addition, a transrectal ultrasound of the prostate is performed.
In the anus, the temperature is usually increased and differs from the temperature of the modes with the mouse by about one degree. When analyzing urine, the indicator of the number of leukocytes is exceeded. The blood tests also highlight some changes, such as the number of eosinophils going down and neutrophil leukocytosis. Sepsis with complications of prostatitis is often observed in immunocompromised patients.
When palpating the perineum, the patient is in pain, the patient has an increase in inguinal lymph nodes. The prostate is enlarged, swollen, and hot to the touch when palpated, and sometimes with heterogeneous seals of inflammation. If the prostate is inflamed, a biopsy will not be done and the infection can spread.
Treatment of prostatitis consists in the use of antibiotics against microorganisms that cause this disease. Antipyretics are also prescribed to lower body temperature and use emollient laxatives to help ease bowel movements. The patient is prescribed a massage, which consists of squeezing the inflamed secretion with your fingers, pushing it out into the ducts, and finally into the urethra. Prostate massage improves blood circulation and has a good effect on the muscle tone of the prostate.
Prevention of prostatitis
To prevent prostatitis, you should initially limit yourself to food and follow a special diet. You need to include in the diet such foods as parsley, asparagus, strawberries. If you like pasta, etc. , these should be tough types. You should also exclude bad habits and alcohol, spicy food. With an exacerbation of the disease, it is very important to exclude sex life.
To prevent prostatitis, it is necessary to exclude all risk factors for its occurrence, namely: adhere to proper nutrition, exclude bad habits and lead a regular sex life, as this will prevent sperm accumulation. Every young man should know that sexual promiscuity is bad for the prostate. An active sex life increases the risk of developing sexually transmitted diseases. Use contraception anyway. Monitor your bowels and use the bathroom regularly. Another important point is work: if it is associated with a sedentary type, then you need physical activity, jogging is also useful, swimming and tennis. Also, do not forget about daily walks in the fresh air, it is very beneficial for the whole body. Hypothermia affects the immune system and at this point the infection progresses. You should be examined by a urologist, even if there are no prerequisites for this.
Timely treatment of a genitourinary infection will help eliminate the cause of the development of prostatitis.
Folk remedies for the prevention of prostatitis are also popular, on the basis of which recipes such as the inclusion of honey, nuts and dried fruits, rich in vitamins and minerals, are distinguished in the diet. Pumpkin seeds and onions, oatmeal and seafood, liver and apples are rich in zinc and therefore have special, important value and great benefits for the prostate. Add the tips above: Empty your stomach completely and avoid constipation. This helps products like kefir, vegetable oil, and vegetable fiber. Separately, it is necessary to mention the benefits of exercises for the intimate muscles.
Exercises to prevent prostatitis are simple and do not require any special adjustment. They can be done anytime, anywhere. Here are a few examples: Move the perineum as if you were pulling the rectum. Tense the muscles of the perineum and try to stop urination. Hold them in this position for as long as possible. While lying down, lift your pelvis and hold it for twenty or thirty seconds. Repeat these movements until you feel pain and fatigue in your buttocks. Such simple exercises are just a plus for your body.





























