What is prostatitisWe analyze the causes of the occurrence, diagnosis and methods of treatment in the article of a doctor, urologist with 28 years of experience.
Definition of disease. Causes of the disease
ProstatitisIs an inflammatory process of prostate tissue, accompanied by pain in the lower back, perineum or pelvic area, as well as disorders in the work of the lower urinary tract.
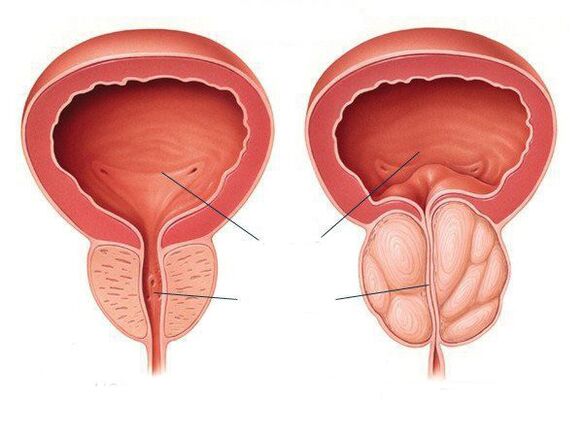
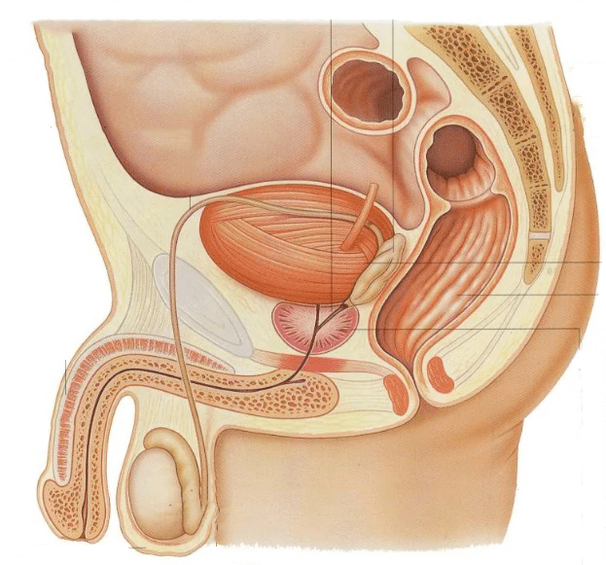
The prostate (prostate) refers to the male reproductive system. It sits in front of the rectum, below the bladder, and surrounds the urethra (urethra). Because of this, when the prostate becomes inflamed, it compresses the urethra, causing various urination problems. The main function of the prostate is to produce secretion (fluid), which is part of the semen and liquefies it to ensure normal sperm motility.
Pathological diseases of the prostate, such as cancer or benign hyperplasia, are more common in elderly patients. Prostatitis differs in that it affects men of all ages, but most often the disease occurs in men of childbearing age (from 8 to 35% of cases).
Prostatitis most often occurs in a urologist's office. It can appear suddenly (acute) or gradually, and its manifestations are constant and long-term (chronic). The chronic form is much more common than the acute. Chronic prostatitis ranks fifth among the twenty most important urological diagnoses.
Prostatitis can either be a disease in its own right or it can be combined with benign prostatic hyperplasia and prostate cancer. In recent years the incidence of prostatitis in the male population has decreased: in 2012 the incidence was 275 per 100, 000 of the population, the primary incidence in 2017 was 203 per 100, 000 of the population.
The reasons for the development of prostatitisare bacterial (infectious) and non-bacterial (non-infectious).Infectious prostatitismost common in men under 35. Most often, this form of the disease is caused by gram-negative microorganisms, especially Enterobacter, E. coli, Serration, Pseudomonas and Proteus, as well as sexually transmitted infections such as gonococci, chlamydia, etc. Very rarely prostatitis can occur due to Mycobacterium tuberculosis. In chronic bacterial prostatitis, the spectrum of pathogens is broader and can include atypical pathogens. It should be remembered that chronic bacterial prostatitis is a polyetiological disease, that is, it can have several causes.
Factors that contribute to the development of inflammationin the prostate:
- sexually transmitted infections;
- Immunodeficiency states;
- Prostate biopsy;
- invasive manipulations and operations;
- Way of life;
- Diarrhea, constipation;
- homosexual contacts;
- frequent change of sexual partners;
- Sedentary lifestyle, etc.
Chronic non-bacterial prostatitisdiagnosed in patients who complain of chronic pain in the prostate area while no infectious (bacterial) agent of the disease was found in them. Despite numerous studies, the cause of this type of chronic prostatitis is not fully understood, but there are some factors that can cause its development:
- increased prostate pressure;
- Pelvic muscle pain;
- emotional disorders;
- Autoimmune diseases (antibodies that fight infection sometimes attack cells in the prostate for some reason);
- physical activity;
- irregular sex life;
- Lifting weights etc.
In some cases, prostatitis can occur after performing transurethral procedures such as urethral catheterization or cystoscopy, as well as after a transrectal biopsy of the prostate.
Although the actual incidence of various types of prostatitis has not been definitively established, the following data are provided:
- acute bacterial prostatitis accounts for about 5-10% of all prostatitis cases;
- chronic bacterial prostatitis - 6-10%;
- chronic non-bacterial prostatitis - 80-90%;
- Prostatitis, including prostatodynia (neurovegetative disorders of the prostate) - 20-30%.
If you experience similar symptoms, contact your doctor. No self-medication - that is dangerous to health!
Symptoms of prostatitis
All forms of inflammationthe prostate, in addition to the asymptomatic, is united by the presence of the following symptoms:
- Lumbar pain;
- Discomfort with intestinal peristalsis;
- Pain in the perineum or pelvic area;
- Disorders in the work of the lower urinary tract.
The main symptoms of the lower urinary tract in prostatitis:
- frequent need to urinate;
- Difficulty urinating, that is, a weak stream and the need to "strain" yourself;
- burning pain or its aggravation when urinating.
In men diagnosed withacute bacterial prostatitisPelvic pain and urinary tract symptoms such as increased urination and urinary retention occur. This can lead to the development of systemic manifestations such as fever, chills, nausea, vomiting, and malaise. Acute bacterial prostatitis is characterized by a sharp onset of the disease with a vivid clinical picture. This is a serious illness.
Men diagnosed withchronic bacterial prostatitisNotice symptoms of a periodic nature that increase and decrease. During an exacerbation, pain and discomfort are noted. Pain sensations are mostly localized at the base of the penis, around or above the anus. Pain can also appear just above the pubic bone or lower back and spread to the penis and testicles. The bowel movement becomes painful too. Sometimes signs of a lower urinary tract infection develop: burning pain and frequent urination, more frequent urge. These symptoms can be confused with the manifestations of acute bacterial prostatitis, but it usually occurs suddenly, chills, fever, weakness, pain throughout the body, lower back, as well as in the genitals, frequent and painful urination, pain with ejaculation. If you experience such symptoms, you need to urgently consult a doctor.
If standard modern research has not found that chronic pain is caused by a pathological process in the prostate, then it is chronic non-bacterial prostatitis, also known aschronic pelvic pain syndrome(the term has been used since 2003). In the presence of chronic pelvic pain syndrome, a man's quality of life is significantly reduced, as this syndrome sometimes leads to various psychological and sexual disorders:
- increased fatigue;
- feeling helpless;
- erectile dysfunction;
- painful ejaculation;
- Pain after intercourse, etc.
With chronic non-bacterial prostatitis / chronic pelvic pain syndrome, there is a feeling of persistent discomfort or pain in the lower back, more often at the base of the penis and around the anus, for at least 3 months. Painful sensations are localized in a "target organ" or several pelvic organs. Most often, with this form of prostatitis, the pain is localized in the prostate (46%).
In chronic prostatitis, sexual disorders have a number of characteristics. First, all components of a man's copulative (sexual) function are disturbed to different degrees: libido, erection, ejaculation. Second, sexual dysfunction occurs mainly in people with a long history (more than 5 years). Third, sexual dysfunction is often the number one reason to see a doctor.
Erectile dysfunction is noted by 30% of patients with chronic prostatitis, mainly due to the psychogenic factor - a catastrophic perception of the disease.
Prostatitis symptoms occur at least once in a lifetime in 50% of men.
Pathogenesis of prostatitis
The mechanism by which prostatitis develops is complex and complex. Many factors are involved in its development. Most cases of acute bacterial prostatitis are caused by a cascade of processes triggered by an ascending urethral infection or intraprostatic reflux.
The penetration of microorganisms into the prostate is possible ascending (through the urethra) or transrectally via the lymphatic route. Diarrhea and constipation in connection with impaired rectal barrier function are considered provoking factors in chronic prostatitis. However, the mechanism by which microorganisms penetrate the prostate is not yet clearly understood.
Urinary tract disease with prostatitis can have the following causes:
- Increasing the tone of the smooth muscles of the prostate urethra by increasing the activity of adrenergic receptors;
- Enlargement of the prostate or narrowing of the urethra resulting in turbulent urine flow, bladder outlet obstruction, and intraprostatic reflux.
In the future there is a violation of the drainage of the prostate ducts, stagnation of prostatic secretions, edema, activation of the arachidonic acid cascade, inflammation and ischemia. A vicious circle of pathological changes forms.
Classification and stages of development of prostatitis
There are 4 main categories (types) of prostatitis.
- Acute bacterial prostatitis(Category I).
- Chronic bacterial prostatitis(Category II).
- Chronic non-bacterial prostatitis / syndromechronic pelvic pain (Category III). Can be flammable (Category III A) or non-flammable (Category III B).
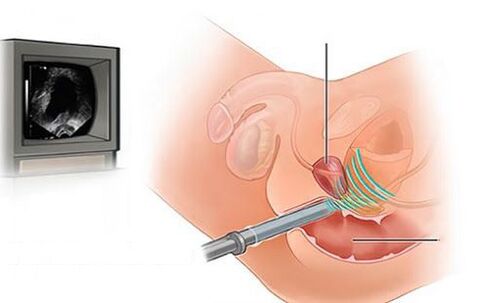
- Asymptomatic inflammatory prostatitis.Histological prostatitis identified by prostate biopsy (Category IV).
Chronic bacterial prostatitisin contrast tospicy,manifests itself as recurrent episodes of exacerbations with the presence or absence of complete remissions between them. Symptoms are usually less severe than those of acute prostatitis.
Classification by the National American Institutes of Health. . .
- Type I.(acute bacterial prostatitis) - acute infection of the prostate: symptoms of the disease appear suddenly. Chills, fever, whole body pain, weakness, lower back and genital pain, frequent, painful urination, pain when ejaculating. Symptoms of acute bacterial prostatitis include blood in the urine and / or semen. It's rare. It is effectively treated with antibiotics.
- II type(chronic bacterial prostatitis) - a chronic or recurrent infection of the prostate: symptoms are the same as those of acute prostatitis, but they come on gradually and are less pronounced. Several courses of antibiotic therapy may be required.
- III type(chronic non-bacterial prostatitis and chronic pelvic pain syndrome): no evidence of infection.
- III A type: Presence of leukocytes in the ejaculate / prostate secretion / third portion of urine after prostate massage.
- III B type: Absence of leukocytes in the ejaculate / prostate secretion / third portion of urine after prostate massage. Lower back and genital pain, frequent urination, difficulty urinating (often at night), burning sensation or pain when urinating and ejaculating. Represent approximately 90% of all prostatitis cases. There are no known causes or clinically proven treatments.
- IV type(Asymptomatic inflammatory prostatitis): Sometimes an increased number of white blood cells. No treatment required. Detected on prostate biopsy.
The lines between the different forms of prostatitis are blurred.
Complications of prostatitis
With inflammatory lesions of the prostate, neighboring organs are involved in the pathological process: the seminal tubercle, Cooper's glands, seminal vesicles and the posterior urethra. The infection can penetrate the prostate and surrounding organs at the same time.
Vesiculitis- Inflammation of the seminal vesicles. The pain is localized in the groin area and deep in the pelvis and radiates to the sacrum. The pain is usually one-sided, as both seminal vesicles are affected to different degrees. Vesiculitis can be asymptomatic. The only complaint from patients may be the presence of blood in the semen. Periodic pyuria (pus in the urine) and pyospermia (pus in the ejaculate) are also noted.
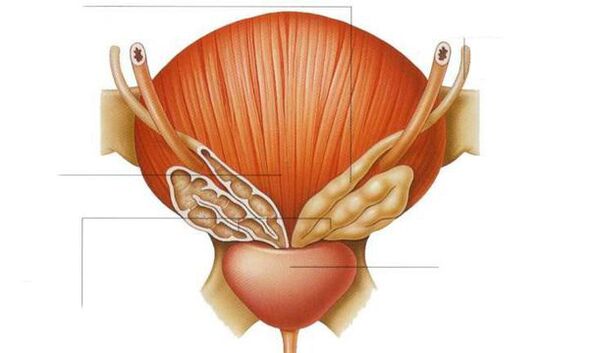
Posterior urethritis, colliculitis (inflammation of the siliar tuberosity). . . In prostatitis, the infection penetrates the spermatic tube, this is due to the proximity of the prostate to the excretory ducts.
Abscess of the prostate.The causative agents of prostatitis can also cause an abscess of the prostate. This is a serious septic (bacterial) disease that is accompanied by weakness, fever, chills with pouring sweat. In some cases, impaired consciousness and delirium are observed. The patient needs hospitalization.
Sclerosis of the prostate (fibrosis). This is a late complication of prostatitis that results from the replacement of prostate tissue with scars (connective tissue degeneration, that is, sclerosis), causing the gland to shrink, decrease in size, and completely lose its function. As a rule, sclerotic symptoms develop long after the inflammatory process in the prostate begins.
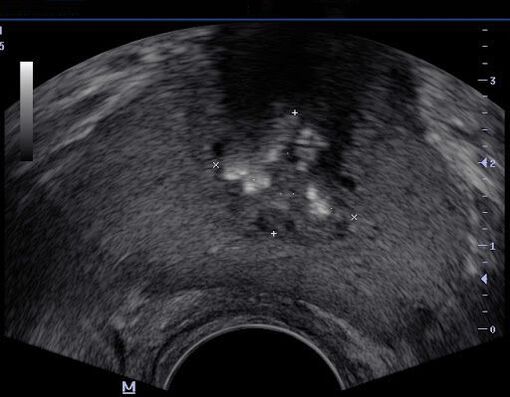
Prostate cysts.These formations can contribute to the formation of stones in the prostate. The presence of an infection in a cyst can lead to a prostate abscess. It is not difficult to diagnose a prostate cyst with ultrasound. They can also be detected with a digital rectal exam.
Prostate stones.They're pretty common. The causes of the disease are not fully understood, but most experts agree that it arises as a result of a persistent inflammatory process in the prostate. Stones are single and multiple, with a diameter of 1 to 4 mm. Large stones are rare. The stones clog the gland, causing the secret inside to stagnate, overstretching the gland and forming separate cysts into which the infection enters. Patients with stones in the prostate constantly struggle with dull pain in the perineum. Painful sensations spread to the glans penis, causing frequent urination, which becomes difficult and painful.
Infertility.Chronic long-term prostatitis primarily reduces the motor function of the sperm and makes them completely immobile. One of the consequences is a violation of their production, the formation of immature spermatozoa with an abnormally changed shape (and fewer in number than before).
Ejaculation disorder.Prostatitis of all forms causes sexual dysfunction. Initially, patients face premature ejaculation, have a normal erection, which then subsides and the degree of orgasm decreases. The prolonged existence of chronic prostatitis contributes to a decrease in the production of male sex hormones and a weakening of the libido.
Erectile dysfunction.The relationship between chronic prostatitis / chronic pelvic pain syndrome and erectile dysfunction has been described. This disorder is particularly painful for men.
Diagnosis of prostatitis
The appearance of the first signs of inflammation of the prostate requires immediate medical attention. The urologist will exclude many diseases with similar manifestations and determine what category (type) the disease belongs to. Before choosing a treatment, a specialist will conduct the necessary examinations and offer an assessment test.
What questions could the doctor ask?
At the appointment, the doctor will definitely indicate: the duration of the clinical manifestations of the disease, the location and nature of the pain, for example, in the perineum, scrotum, penis and inner thigh; Changes in the nature of the semen (the presence of pus and blood).
At the reception, the urologist offers to fill out special questionnaires, including the index of symptoms of chronic prostatitis.
The patient should ask questions to the doctorabout what tests and studies to do, how to prepare for what treatment to prescribe, and where to get more information about the disease.
Chronic bacterial prostatitis is diagnosed if symptoms persist for at least three months.
The survey includes:
- Digital rectal examination of the gland to determine the extent of prostate enlargement and its consistency.
- Tests of secretions from the prostate, urine and / or ejaculate.
- Identification of a genitourinary infection.
- Ultrasound examination of the urinary tract (kidneys, prostate, bladder with residual urine determination).
- Urodynamic study.
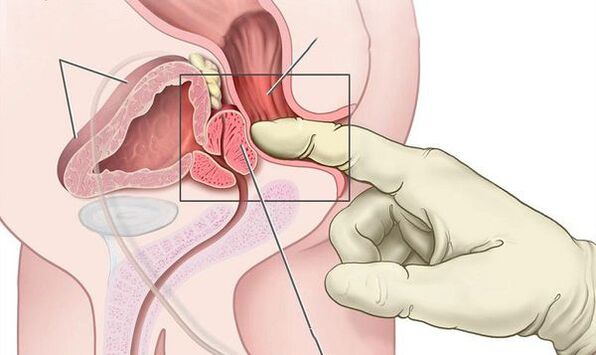
For acute bacterial prostatitis, a digital rectal exam can reveal a swollen and painful prostate. Prostate massage is contraindicated as it can lead to bacteremia and sepsis.
The most important examination when examining patients with acute bacterial prostatitis is the culture of prostate secretions. Quantitative culture and microscopy of urine samples and prostate secretions obtained after massaging the prostate are still important methods for categorizing chronic prostatitis.
Androflor - a comprehensive study of the microbiocenosis of the genitourinary tract in men by PCR. Allows you to determine the qualitative and quantitative composition of the microflora. It is used to diagnose and control inflammatory infectious diseases of the genitourinary system.
After determining the cause of the disease, the doctor will recommend treatment. It should be noted that with standard methods, an infection can be detected only in 5-10% of cases, which ultimately leads to prostatitis.
What is the relationship between prostatitis, prostate specific antigen (PSA) and prostate cancer?
Measurement of total PSA and free PSA in prostatitis does not provide additional diagnostic information. It is known that the level of prostate-specific antigen (PSA) increases in 60% and 20% of patients with acute and chronic bacterial prostatitis, respectively. After stopping treatment, the PSA level drops in 40% of patients. PSA is not considered a specific marker for prostate cancer because the PSA level can be increased in benign prostatic hyperplasia and prostatitis.
Treatment of prostatitis
The leading role in the treatment of pathology is attributed to drug therapy.
Treatment with alpha1 blockers
Alpha1 blockers are prescribed to patients who complain of difficulty urinating. These medicines help make urination easier and relax the muscles of the prostate and bladder. Some patients are prescribed drugs to lower hormone levels, which can help shrink the gland and relieve discomfort. Muscle relaxants can help relieve pain caused by an edematous prostate that puts pressure on nearby muscles. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help with pain.
Standard antibiotic therapy in most cases does not lead to a reduction in the number of flare-ups, so an integrated approach is often used and also prescribedAuxiliary drugs: Biostimulants, extracts of various plants and insects and their biological components that may be in the formrectal suppositories. . . Despite the large arsenal of drugs, the effectiveness of their use remains insufficient.
Physiotherapy in the treatment of prostatitis
In the case of chronic prostatitis of categories II, III A and III B, physiotherapeutic methods can also be used:
- Massage of the prostate (prostate);
- Laser therapy;
- Microwave hyperthermia and thermotherapy;
- electrical stimulation with modulated currents from cutaneous or rectal electrodes;
- Acupuncture (acupuncture).
The effectiveness and safety of these treatments is still being investigated. Also used to treat prostatitisFolk methods, e. g. B.Hirudotherapy.The effectiveness and safety of this method of treating prostatitis has not been established.
Stem cell injection
Cell therapy (stem cell injections) in the treatment of prostatitis is currently a promising technique in the early stages of development. For the injection of stem cells into the prostate, there are currently only hypotheses about their mechanisms and empirical data from individual research groups.
Surgical treatment of prostatitis
Surgical methods are used only to treat complications of prostatitis - abscess and suppuration of seminal vesicles.
The treatment of chronic pelvic pain syndrome requires separate consideration. Asymptomatic inflammatory prostatitis (Category IV) should not be treated unless the patient plans to have prostate surgery. In this case, the patient is given prophylactic antibiotic therapy.
Diet and lifestyle in prostatitis
No special diet is required for prostatitis, but eating lots of vegetables, lean meat, and dairy products will improve bowel function. It is important to get enough fiber, foods rich in vitamin E (wheat germ, corn oil, etc. ), sugar should be replaced with natural honey. Proper nutrition for prostatitis can improve bowel function and reduce the chance of relapse or speed recovery. It is recommended to follow a healthy lifestyle, drink more fluids, and limit caffeine and alcohol.
Forecast. prophylaxis
Acute prostatitis often becomes chronic, even with timely and appropriate treatment.
Full recovery is not always possible, but with the right consistent therapy and the recommendations of the doctor, discomfort and pain can be eliminated. IndependentlyTreatment of prostatitis at homecan be dangerous and lead to complications.
Not all cases of prostatitis can be identified as a cause, but there are a number of steps you can take to prevent prostatitis from developing. The same steps can help control existing symptoms:
- Drink enough fluids. Drinking plenty of fluids leads to frequent urination, which makes it easier to flush out infectious agents from the prostate urethra.
- Empty your bladder regularly.
- Avoid irritation of the urethra. Limit your intake of caffeine, spicy foods, and alcohol.
- Reduce the pressure on the prostate. Men who ride bicycles often need to use a split seat to relieve the prostate area.
- Remain sexually active.





























